Age-related Macular Degeneration
Age-related macular degeneration (AMD) occurs as a result of deterioration of the central portion of the retina, called the ‘macula’. These changes in the macula can lead to a significant loss of central vision (visual acuity).
AMD is the leading cause of severe vision loss in the developed world in people over the age of 50. In North America approximately 15 million people currently have the “dry” form. This represents 85-90% of all AMD patients. Another 1.7 million have the “wet” type which constitutes 10-15% of all AMD cases.
Although the precise cause remains unknown, it results in deterioration, or breakdown of the macula — the small part of the retina that enables people to see fine details and colour. In the early stages, a patient may have no symptoms. With progression of the AMD, symptoms may include distortion or warping of straight lines, a decreased ability to read and see detail, and decreased brightness of colours. As the disease advances, a patient may notice gradual or sudden loss of central vision, and dark or blurry areas in the centre of vision (scotomas).
There are two basic forms of macular degeneration — known as 'dry' or non-neovascular; and 'wet' or neovascular.
In early stages of dry AMD, the hallmark change is drusen—pale yellow accumulations formed beneath the retina . Individually drusen are usually harmless, but as they accumulate, dry AMD can progress. Atrophic areas (areas of atrophy or thinning) in the retina may develop; if the atrophic area is significant and with sharp borders, it is termed geographic atrophy (GA).
GA is the advanced form of dry AMD, and is usually associated with loss of central vision.
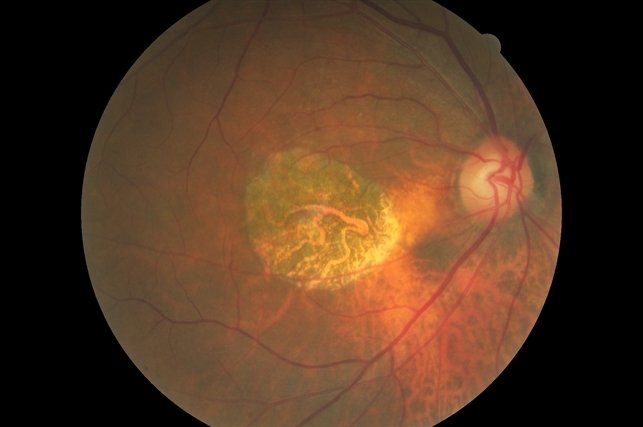
In wet AMD, there is a sudden or gradual decrease in visual acuity, blind spots in the center of vision, and distortion of straight lines. The hallmark of wet AMD is choroidal neovascularization (CNV) (Figure 2).
CNV occurs when abnormal blood vessels grow beneath the retina; these can bleed or leak and cause a distortion of the retina’s structure. Ultimately, the CNV can turn into a thick fibrotic scar (disciform scar) that replaces the normal structure of the macula and leads to permanent loss of central vision.
While the wet form occurs in only about 10 - 15% of all macular degeneration cases, it causes much more damage than the dry form.
Population-based studies have revealed a number of risk factors:
Age: is the greatest factor. In developed countries, 10% of people over the age of 65 years and 25% over the age of 75 years have AMD.
Female gender
Hypertension
Elevated cholesterol levels
Cardiovascular disease
Positive family history of AMD
Cigarette smoking
Hyperopia (far-sightedness)
Light iris colour
Racial origin: a ten year longitudinal study found the highest prevalence in whites (5.4%), lowest in African Americans (2.4%), and intermediate in Hispanics (4.2%) and Asians (4.6%).
Genetics may play a role. Numerous mutations within certain genes may affect biochemical pathways that contribute to the development of AMD however this area is in the early stages of research and understanding.
Diagnostic Testing
In diagnosing Macular Degeneration, Dr. Uniat performs a complete clinical examination with the slit-lamp microscope and indirect ophthalmoscope. Several diagnostic tests may be performed at her office including:
Optical Coherence Tomography scan
Fluorescein angiography
Indocyanine green angiography
Treatment of Macular Degeneration
WET AMD
Over the last 15 years treatment for Wet AMD has been dramatically transformed with the scientific discovery of a biochemical family of naturally occurring compounds in the human body named vascular endothelial growth factor (VEGF).
VEGF plays a significant role in the formation and growth of abnormal new blood vessels beneath the macula—known as neovascularization—that can lead to wet AMD. These new blood vessels are very fragile, leak fluid, and can bleed leading to deterioration of central vision.
Anti-VEGF drugs have been developed to help stop neovascularization and preserve vision for AMD patients. There are currently 5 different anti-VEGF drugs:
Avastin® (bevacizumab)
Lucentis® (ranibizumab)
Eylea® (aflibercept)
Beovu® (brolucizumab)
Vabysmo (faricimab)
There is also an extended release device (Susvimo) that can be implanted in the operating room and refilled in the office every 24 weeks with a concentrated form of Lucentis. Susvimo is not available in Canada.
Wet AMD cannot be cured, but its progression may be blocked with the use of intravitreal (in-the-eye) anti-VEGF injections. These injections may preserve, and even recover, vision. Local anesthetic eye drops are given before the injections to numb the eye and minimize discomfort.
There are 3 anti-VEGF treatment regimens:
Pro re nata (PRN) or “treat and observe”—patients are treated with three initial monthly injections, followed by treatment as needed.
“Treat and extend”—after 3 initial monthly injections, the time between treatments is gradually increased until wet AMD is stabilized.
Monthly injections.
Before the first anti-VEGF drugs were introduced, wet-AMD patients were treated with laser photocoagulation or photodynamic therapy (PDT). These modes of treatment were far less successful and patients commonly continued to show progression of disease and vision loss.
Anti-VEGF drugs have greatly improved wet-AMD treatment since 2005; patients today have a much better chance of maintaining their central vision so they can read, drive, recognize faces, and live normal lives.
These anti-VEGF medications are very costly and in 2014, the retina specialists in Alberta, together with the Government of Alberta, developed the RAPID program to cover the cost of these drugs. It has been very successful both in helping to maintain vision and as a cost saving measure.
DRY AMD
No current treatment can prevent visual loss for patients with GA (the advanced form of dry AMD). However, the Age-Related Eye Disease Studies (AREDS), conducted by the National Eye Institute, have found that a nutritional supplement formula may delay and prevent intermediate dry AMD from moving to the advanced form.
The AREDS supplement formula, which is widely available over the counter, contains:
Vitamin C
Lutein
Vitamin E
Zeaxanthin
Zinc
Extensive research has recently developed a drug which attacks another biochemical pathway, the complement system, which has been shown to be involved in the development of dry AMD. Recent studies have shown a very positive effect in treating dry AMD.
Although patients with either form of AMD can experience a progressive decrease in visual acuity, they will almost never be completely blind.
Image above is an example of blurring and loss of definition with Macular Degeneration
Hover over image above to see visual disruption from Macular Degeneration
Advanced Dry Age-Related Macular Degeneration
Images above and below show Wet Age-Related Macular Degeneration with Hemorhhage
Macular Degeneration with Drusen